We give joy of life
After years with a chronic wound, thanks to the cold plasma therapy I can I can be active again and enjoy life!
Sandra Henn
CPT® patient
After years with a chronic wound, thanks to the cold plasma therapy I can I can be active again and enjoy life!
Sandra Henn
CPT® patient
"By offering CPTpatch therapy, we have established ourselves as an innovative treatment center and significantly increased the number of patients."
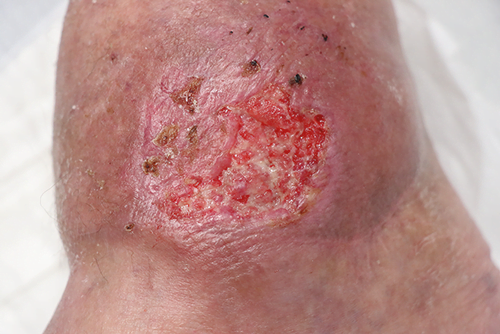
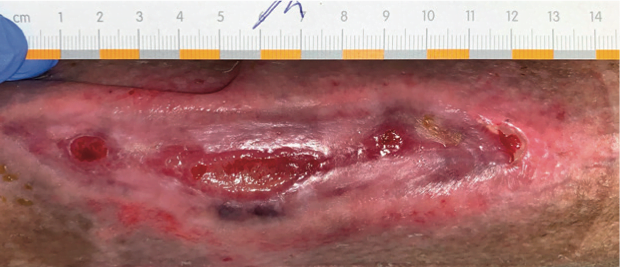
The initial presentation of the patient to our outpatient clinic was due to a persistent wound healing disorder of the right lateral malleolus after impact trauma. The probable cause of the delayed wound healing was peripheral arterial occlusive disease with occlusion of the anterior tibial artery.
Initially, surgical wound debridement was performed with subsequent defect coverage with a peronaeusbrevis muscle flapplasty and a split-thickness skin graft. After the patient was discharged with closed wounds, a wound infection occurred under ambulatory care with ischemic wound conditions resulting in chronic wound healing disorders and extensive split skin loss. In the course of the renewed inpatient stay, surgical wound cleansing was performed, which was ultimately insufficient for healing.
To improve the wound situation, we therefore started cold plasma therapy during the inpatient stay.
The CPT®patch, which is used with the CPT®cube, was atraumatically attached to the wound area to be treated with the self-adhesive edge. The active wound dressing allows the generation of a planar, cold atmospheric pressure plasma in a non-invasive setting.
With increasingly improved wound conditions, therapy was continued in an outpatient setting. During the first four weeks of treatment, therapy was performed 3 times per week. (Fig. 2).
Each treatment session had a duration of two minutes. In the last three weeks of treatment, the frequency was reduced to two applications per week. Each plasma treatment was followed by covering the wound with commercial dressings and elastic compression wrapping of the affected lower leg.
After just a few applications, we were able to record a positive effect on wound healing. Starting from an initial wound size of 4 cm2, the defect was only 0.75 cm2 four weeks after treatment (Fig. 3). Six additional treatment sessions reduced the wound size to 0.08 cm2. The remaining defect was dry and free of irritation.
In addition to the increasing reduction of the wound area, we also registered a significant decrease in wound coatings. Before the start of cold plasma application, a Staphylococcus aureus colonization was detected in the microbiological examination of the wound swab. In the further course of treatment, no further germ spectrum was detectable. Cold plasma therapy was well tolerated and showed no local or systemic side effects.
Due to the enormous improvement in the wound situation after cold plasma application, we were ultimately able to dispense with further wound debridement and subsequent extensive reconstruction of the soft tissue defect with a free flap reconstruction in the old patient. Despite exposed bony portions, the wound showed a good granulation tendency after cold plasma application (Fig. 4).



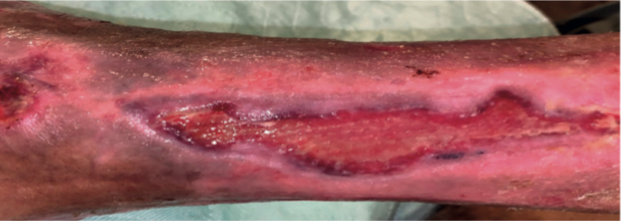
66-year-old patient, previous diseases: pAVK of the pelvic-leg type bds, Z.n necrotizing fasciitis foot and lower leg and Z.n multiple plastic reconstructive procedures on the left lower leg.
Due to a soft tissue defect on the right lower leg, the patient underwent soft tissue reconstruction with a free flap. In the postoperative course, pressure damage led to ulceration, which was surgically repaired and treated with a split skin graft.
Skin transplantation failed to achieve complete re-epithelialization, and part of the graft was lost. In order to stabilize the wound situation, we therefore started a therapy with cold plasma. Regular (initially at least 2x/week) cold plasma treatment of the wound was performed over a period of three months. During this time, the patient was able to continue working.
Frequency of cold plasma treatment with the CPT®patch 2 x to 3 x weekly.
Supportive 3x/week Dressing change with grease gauze (Lomatuell, polyhexanide gel), compresses and an elastic wrap.



-Ulcus cruris
-Necrosis foot/toe right
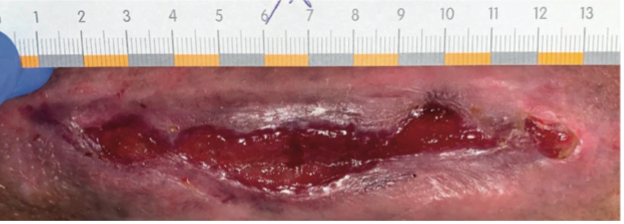
The initial presentation to our clinic was due to chronic ulcerations on both lower legs caused by chronic venous insufficiency.
Initially, surgical wound care was performed with wound debridement and subsequent defect coverage of the soft tissue defects with a split skin graft. The patient was discharged from the inpatient treatment with almost completely healed split skin grafts.
However, in the course of further outpatient treatment, the wound situation on the foot now worsened.
The patient did not wish to have the wound surgically repaired. Under conservative wound treatment with regular dressing changes (every 2 days: Lomatuell, PVP iodine, compresses, absorbent cotton, elastic wrapping), the wound showed no significant healing tendency. Hoping to improve the wound situation and stimulate the healing process, we started cold plasma therapy additively after two debridements.
Regular (initially min. 1 x/week) cold plasma treatment of the wound was performed over a period of two months.
The development of the wound situation can be seen in the attached picture material and speaks for itself.




- Z.n. medial infarct r. 12/2020 with persistent hemiparesis on the left side with occlusion of the common carotid artery on both sides
- Occlusion of right subclavian artery, bypass truncus brachiocephalicus to right axillary artery 12/2020
- Upper GI bleed Forrest Ib with clipping 02/2021
- Ulcus cruris mixtum right calf
- Urinary and fecal incontinence
- Cognitive impairment
- COVID infection
- Respiratory insufficiency
- Positioning must be constantly controlled because patient is very restless
61 year old male patient, lying in the center for respiratory care and hospitalized there. The patient has a lack of understanding of the disease, a weakened immune status, cachexia, consumptive underlying disease, cognitive impairment and is completely immobile.
The patient was admitted from a hospital in Berlin with an existing venous leg ulcer. This had already existed for several weeks at home.
Initial situation on 30.11.: Wound therapy so far: Mechanical cleaning with NaCl and sterile compresses, covering with Allevyn Gentle. Dressing changes every 4 days and as needed. No compression because mixed ulcer and arterial vascular status are very impaired.

- Cerebral arterial occlusive disease with high-grade ACI stenosis on the right
- stage II decubitus at the sacrum
- condition after alcohol abuse
- condition after pneumonia
- Leg amputation on both sides
- Urinary and fecal incontinence
- Unstable general condition
- Poor nutritional status
The 56-year-old male patient was cared for in a rehabilitation clinic. He had a long-standing alcohol and drug problem. This resulted, among other things, in a weakened immune status and a lack of understanding of the patient. He is completely immobile, as both legs had to be amputated due to pAVK (right leg 1/2021, left leg 3/2021). Wound treatment was mechanical. Daily dressing changes were performed with absorbent dressings and fixation plasters. Movement promotion took place with the support of the necessary aids. The patient was positioned on the TOTO-Frontier Medical repositioning system.
Fig. 1
Before starting cold plasma therapy, this grade 2 cross-bone decubitus measuring 6.3 x 4.8 x 0.4 cm had been in a stagnant stage for 6 weeks. To activate wound healing, we tried therapy with a collagenase product for 4 weeks. Unfortunately, the patient did not respond. The supply of dressing materials then also led to a polyacrylate allergy and a clearly reddened wound environment, which then prompted us to implement a new therapy variant.
Fig. 2 and 3
The CPT®patch made of atraumatic material is placed on the decubitus and connected to the CPTcube. The finger presses on the rima ani to ensure a closed chamber so that the cold plasma can be fully applied and cannot escape. Once switched on, it generates a flat, cold atmospheric pressure plasma to promote wound healing even of locally infected tissue defects. Even multi-resistant germs are killed. The treatment is rather painless for the patient and is completed after 2 minutes. For safety, the CPT device automatically returns to standby mode after the specified treatment time. An "overdose" can thus be safely ruled out.
In addition, wound therapy consisted every 3 days of: Cleaning with saline, covering with a polyurethane foam dressing with silicone coating (Biatain® Silicone).
The parts of the body considered for application are mainly the extremities and the trunk.
Fig. 4
After 2 cold plasma treatments, redness of the surrounding skin and wound edges continued to decrease with granulation tissue at the base of the wound and decreasing exudation.
Fig. 5
On 13.12., the skin surrounding the wound was already peeling off, with well perfused granulation tissue and moderately serous exudation.
Fig. 6
shows almost complete epithelialization with well perfused wound conditions and decreasing wound exudation. The patient reported no pain before, during and after treatment.
Unfortunately, the respiratory condition of the multimorbid patient deteriorated again and so did the wound conditions. Thus, unfortunately, a complete closure could not take place.
Cold plasma therapy can be an alternative for stagnant chronic wounds. In addition to promoting cellular activity, there is also a reduction in germs on the wound. Blood flow is stimulated and we saw increasing exudation after 4 weeks of cold plasma therapy and 5 applications. Superficial skin lesions were epithelialized and even the slightly deeper wound areas showed good granulation and significant wound reduction (wound size 15 mm2). With a PU foam adapted to the exudation and the stool drainage Hyghtec®, we were able to achieve good protection of the wound against secondary infection over the period of 4 weeks.






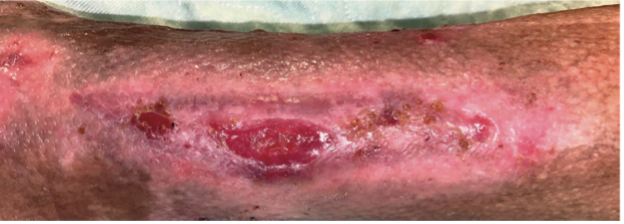
- Ulcus cruris venosum due to insufficiency V. saphena parva at recurrence, Z.n. CVE with crossectomy and stripping V.saphena parca 10 years ago (wound colonization with Excherichia coli Pseudomonas aeruginosa)
- Z.n Tinea pedis, arterial hypertension, polyarthritis, allergies to penicilling, amonopenicillins, cephalosporins, carbapenems, monobactams, antibiotics, novaminsulfone, napproxen, diclofenac.
- The wound had been managed with traditional/modern wound care for approximately 6 years by then, and three hospitalizations were required.
The patient 56 y.o. presented with increasing ulceration, redness and swelling in the area of the right lower leg distal medial 10 x 8.5 cm in size for further therapy. Sonography is performed.
Here, extensive recurrent varicosis of the saphenous vein with correnal recurrence is found. Partial saphenous vein with reflux, lateral varicosis,
Insufficiency of the MAY perforaris. In the area of the deep system (VHS,V.popl.) partial reflux a.e. is also found due to correnal insufficiency.
The patient was treated with the CPT®patch 2-3 times per week in four treatment intervals. The wound size at the beginning approx. 9.5 x 6.3 cm after more than 6.5 years of treatment in 12 weeks of individual therapy could be closed sustainably with the CPT®patch.
Complementary wound care during the treatment phases included dressing changes (from daily to approximately every 4-5 days), use of gauze compresses, Octenisept, compression therapy, and compression stocking.
The patient, who was not mobile at the beginning of the treatment and was struggling with severe pain, is mobile and pain-free after treatment with the CPT®patch. The patient's quality of life has increased significantly.
The patient was in very poor psychological condition after several years of immobility and lack of ability to work, which improved significantly due to good treatment results and regained mobility.
The patient is back to work, pain-free and has regained her quality of life thanks to the successful treatment with the individual therapy with the CPT®patch.



